Colonoscopy
Endoscopic evaluation of the colon and terminal ileum with precision and safety.
Theodoros Argyropoulos, M.D., M.Sc., Ph.D.
Senior Registrar in Gastroenterology, “G. Gennimatas” General Hospital
Scientific Director, Gastroenterology Department – Affidea Peristeri
Contents
What is colonoscopy?
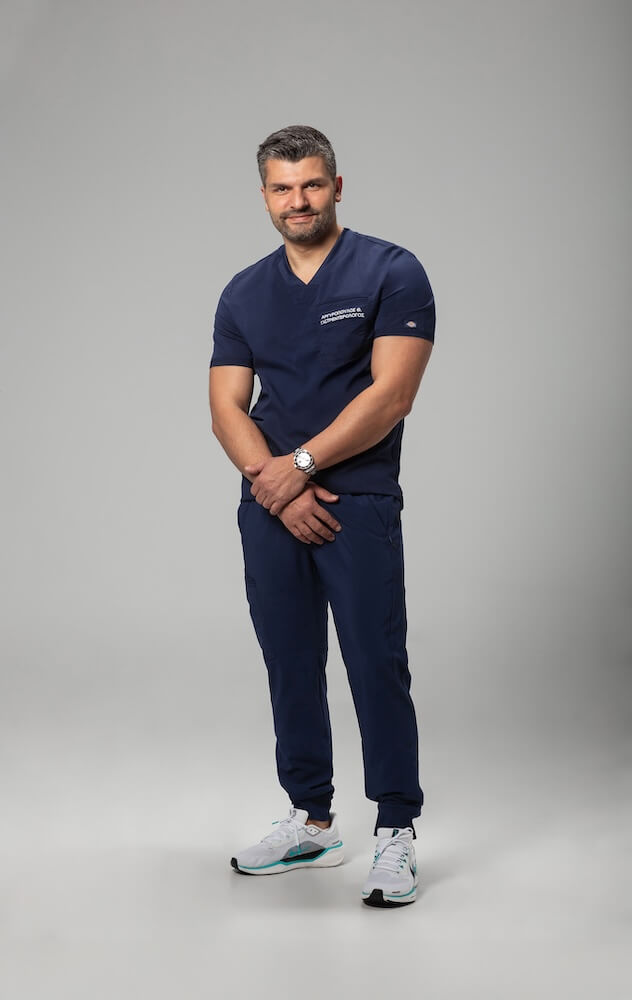
Colonoscopy is an endoscopic examination that allows direct evaluation of the colonic mucosa and, when needed, the terminal ileum. Using a thin, flexible high-definition endoscope, the physician detects and treats lesions such as polyps, inflammation, ulcers, or bleeding sites. Colonoscopy is a safe, painless routine procedure that can easily, promptly, and effectively prevent serious health complications—and ultimately save lives.



When is colonoscopy performed?
Preventive screening (screening)
From the age of 50 (or earlier in high-risk groups: family history, IBD, etc.).
Based on medical evaluation, the frequency of re-examination is determined.
Diagnostic indications
- Blood in the stool.
- Change in bowel habits (recent diarrhea/constipation).
- Iron-deficiency anemia, unexplained weight loss, abdominal/rectal pain.
- Findings from imaging studies (CT/MRI/PET) requiring endoscopic evaluation.
- History of polyps, cancer, or IBD (ulcerative colitis/Crohn’s disease).
- Abdominal pain or rectal pain.
Therapeutic interventions during the procedure
- Polypectomy / removal of precancerous lesions.
- Hemostasis of bleeding lesions.
- Biopsy sampling for histological examination.
- Advanced techniques (e.g., EMR, when indicated).
What preparation and diet should I follow before colonoscopy?
-
Bowel cleansing with a special solution, according to written instructions.
-
Diet: usually restrictive in the days prior; on the day before the procedure, clear liquids are preferred (you will receive a detailed plan).
-
Medication: inform your physician about anticoagulants/antiplatelet drugs, antidiabetic medication, iron supplements, etc. Adjustments may be required.
-
A companion on the day of the procedure (due to sedation) and avoidance of driving afterward.
- Download Preparation Instructions
How is the procedure performed?
Colonoscopy is performed in a specially prepared and sterile environment, with the administration of mild intravenous sedation so that the patient feels comfortable, without pain or anxiety. The gastroenterologist gently inserts the colonoscope—a thin, flexible tube equipped with a high-definition camera—through the rectum, gradually advancing it along the colon and, when required, into the terminal ileum.
During the slow withdrawal of the endoscope, a detailed inspection of the mucosa is carried out to identify any potential lesions, such as polyps, inflammation, or ulcers. If necessary, the physician may take biopsy samples—small tissue fragments sent for histological analysis by a pathologist, to determine whether inflammation, adenoma, or malignancy is present.
Additionally, if polyps are detected, they can be removed during the same procedure through a simple technique known as polypectomy.
The total duration of colonoscopy typically ranges between 30 and 45 minutes, and thanks to sedation, the procedure is painless, safe, and well tolerated by the patient.
After Colonoscopy
-
Post-procedure Instructions
- A short stay in the recovery area until the effects of sedation have worn off.
- Do not drive or operate machinery for the rest of the day.
- Mild bloating or gas is common and will resolve.
- Diet: typically a gradual return to your usual diet (you will receive personalized instructions).
- Contact your physician immediately if you experience severe abdominal pain, fever, persistent vomiting, or significant bleeding.





What does it show?
- Polyps/adenomas, neoplasms.
- Inflammation (IBD), diverticula, vascular lesions.
- Sources of bleeding or anemia.
- Possibility of therapeutic intervention at the same time (e.g., polypectomy, hemostasis).
Cost & Duration
- Colonoscopy lasts approximately 30–45 minutes, depending on the findings and any interventions (e.g., polypectomy). The cost depends on:
- the type of procedure (diagnostic or therapeutic),
- the facility where it is performed,
- as well as the fees of the anesthesiologist and the pathologist.
- In the private sector, this is a specialized procedure, and the fee is determined by the physician’s experience and the specific services included.
Yes. When there is an indication to examine both the upper and lower digestive tract, the procedures can be performed in the same session—typically with gastroscopy first, followed by colonoscopy under the same sedation—for comfort and time efficiency.
Side Effects & Complications
Colonoscopy is a well-established and safe procedure. Rarely, the following may occur: • Bleeding (mainly after polypectomy). • Perforation. • Reactions to sedation. • Abdominal pain that is more intense than gas-related discomfort or cramps. • Bloated and firm abdomen. • Vomiting. • Fever. • Passing a large amount of blood from the rectum (especially after polyp removal).

Dr. Theodoros Argyropoulos’ team follows ESGE/UEG protocols for maximum safety.
Frequently Asked Questions (FAQ)
Why should I undergo colonoscopy?
Colonoscopy is the most important preventive examination for the early detection and diagnosis of conditions such as polyps and colorectal cancer. These conditions can be fully treated when identified in time.
Additionally, the procedure allows for simultaneous treatment, such as the removal of polyps (polypectomy), cauterization of angiodysplasias, or other endoscopic interventions.
Beyond cancer, colonoscopy can diagnose inflammation, diverticula, and causes of bleeding in the colon.
How should I prepare for colonoscopy? What diet is required?
Your doctor will provide detailed instructions a few days before the procedure. Proper bowel preparation is essential for reliable results.
You will need:
A special diet for 2–3 days before the examination.
Allowed: meat, fish, chicken, boiled egg, potatoes, rice, pasta, compote, chamomile tea.
Avoid: fruits, vegetables, legumes, whole-grain foods, fried foods, dairy products.Adequate hydration with water or non-carbonated juices.
Administration of a laxative solution, according to your doctor’s instructions, to ensure complete cleansing of the colon.
Proper preparation is crucial for the accuracy of the examination.
Is colonoscopy painful?
No. Thanks to the administration of mild sedation, the procedure is completely painless and well tolerated by the patient.
When will I receive the results?
No. Thanks to the use of mild sedation, the examination is completely painless and well tolerated by the patient.
Macroscopic findings are communicated immediately after the procedure, while biopsy results are available within a few days, depending on the laboratory.
How often should it be done preventively?
What should I eat after colonoscopy?
A normal diet is usually allowed, with a gradual return to your regular eating habits. Your doctor will provide personalized instructions depending on your case.
Can I work or drive afterward?
Early diagnosis saves lives and allows every condition to be treated before it progresses.
If you are experiencing intestinal discomfort, blood in the stool, or if you have reached the age for preventive screening, do not delay your colonoscopy.
With modern endoscopic technology and the expertise of Dr. Theodoros Argyropoulos, the examination is performed painlessly, safely, and with precision.