Ulcerative Colitis
Theodoros Argyropoulos, M.D., M.Sc., Ph.D.
Consultant Gastroenterologist, GNA “G. Gennimatas”
Head Gastroenterology Department, Affidea Peristeri
What is Ulcerative Colitis?
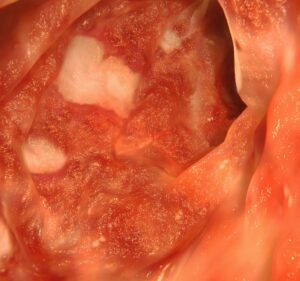
Ulcerative Colitis is a chronic inflammatory disease of the large intestine belonging to the Idiopathic Inflammatory Bowel Diseases (IBD). The inflammation always starts from the rectum and spreads continuously upward, affecting the colon over a larger or smaller extent. The disease causes superficial ulcers in the intestinal mucosa, leading to bloody diarrhea, abdominal pain, and weight loss. It follows a course of relapses and remissions, and the progression differs from person to person.


Symptoms
The most common symptoms of Ulcerative Colitis include:
- Persistent diarrhea with blood or mucus
- Abdominal pain or cramps, mainly in the lower left quadrant
- A sense of urgent need to defecate (tenesmus)
- Loss of appetite and weight
- Weakness and fatigue
- Fever or low‑grade fever during flare‑ups
- Anemia due to chronic blood loss
- Swelling and pain in hips and knees
- Swelling and pain in the eyes, skin, or lungs
In severe cases, the disease may lead to toxic megacolon — a rare but dangerous complication that requires immediate medical attention.
Causes & Risk Factors
The cause of Ulcerative Colitis remains multifactorial. Genetic, immunological, microbial, and environmental factors are involved. Key mechanisms include:
- Immune system dysfunction: the body mistakenly attacks intestinal cells
- Genetic predisposition: increased risk if there is a family history of IBD
- Microbiome imbalance: reduction of “good” gut bacteria
- Environmental factors: pollution, western diet, stress
Risk factors:
- Age: often begins between ages 20–40
- Non‑smokers (paradoxically, the disease is less common among smokers)
- Non‑steroidal anti‑inflammatory drugs (NSAIDs) – may trigger flare‑ups
- Family history of IBD or autoimmune diseases

How is it Diagnosed
Diagnosis of Ulcerative Colitis requires a combination of clinical, laboratory, and endoscopic examinations, since there is no single test that can confirm it alone. Key diagnostic steps:
- Colonoscopy with biopsies — the fundamental examination for confirming the disease, allows direct inspection of the colon’s mucosa and sampling for histological analysis.
- Blood tests — to check inflammation markers (CRP, ESR), hemoglobin, and iron levels for possible anemia.
- Stool tests — fecal calprotectin and lactoferrin can be used to assess inflammation activity.
- Imaging (CT or MRI) — to evaluate the extent and possible complications such as abscesses or bowel dilation.
- Differential diagnosis — Ulcerative Colitis must be distinguished from Crohn’s disease and infectious colitis.
Special endoscopic procedures:
- Sigmoidoscopy — examines the left colon and rectum; used for quick evaluation in acute phases.
- Colonoscopy — examines the entire colon using a thin, flexible endoscope inserted through the rectum up to the cecum (lower right abdomen).
The presence of continuous inflammation, ulcers or bleeding starting from the rectum is a diagnostic indication of Ulcerative Colitis.
Treatment
Treatment aims to reduce inflammation, maintain remission, and improve quality of life. Options include:
-
Medications
- Aminosalicylates (5‑ASA, mesalazine) — first‑line therapy
- Corticosteroids — for short‑term use during flare‑ups
- Immunosuppressants (azathioprine, mercaptopurine) — for maintenance
- Biologic agents (anti‑TNF, anti‑integrin, anti‑IL12/23) — for moderate or severe disease
- JAK inhibitors — newer treatments for resistant cases

-
Diet & lifestyle adjustments
- Avoid spicy, fatty food and caffeine
- Ensure sufficient hydration and protein intake
- Stop smoking and alcohol
- Manage stress and psychological burden

Possible Complications & Follow‑up
- Anemia due to chronic bleeding
- Toxic megacolon
- Bleeding or bowel perforation
- Increased risk of colorectal cancer after 8–10+ years of disease, especially in patients with pancolitis or prolonged active inflammation
- Extra‑intestinal manifestations: arthritis, skin rashes, uveitis
- Regular colonoscopy every 1–2 years is fundamental for surveillance and early detection of precancerous lesions.

Ulcerative Colitis & Colorectal Cancer
- The risk of developing colorectal cancer is
- 2–3 times higher than the general population
- especially in patients with extensive colon involvement or long-standing active disease
- Early detection via high-definition endoscopy or chromoendoscopy allows timely identification of dysplasia and preventive interventions.
Living with Ulcerative Colitis
Although Ulcerative Colitis is chronic, it is manageable. With appropriate treatment and follow‑up, patients can lead a normal social and professional life.
The goal is:
- Remission without symptoms
- Mucosal healing
- Normal daily functioning
Psychological support and dietary guidance play a crucial role in disease management.
If you experience persistent diarrhea, abdominal pain, or blood in your stools, early assessment by a specialized gastroenterologist is critical. Contact Dr. Argyropoulos Theodoros for a full evaluation and a personalized therapy plan.

Frequently Asked Questions
Is it normal to have blood in stool?
No. Blood in the stool is a sign of intestinal inflammation and requires prompt medical evaluation. The presence of blood is among the most characteristic symptoms of Ulcerative Colitis.
Can Ulcerative Colitis be cured completely?
No — it is a chronic inflammatory condition. However, with the right therapy and regular monitoring, full remission without symptoms is achievable, allowing a normal daily life.
Can I get pregnant if I have Ulcerative Colitis?
Yes, provided the disease is in remission. The doctor will adapt the medication regimen to ensure safety during pregnancy. Prenatal counseling is recommended before conception.
Do I need to take medications forever?
Maintenance therapy is usually necessary to prevent flare‑ups and complications. Consistent adherence to medication and regular check‑ups can ensure long-term stability.
Is Ulcerative Colitis hereditary?
Yes, there is a strong genetic predisposition. If a family member has IBD, the risk is significantly increased compared to the general population. That doesn’t mean the disease will definitely occur, but increased surveillance and prevention are advised.
Is Ulcerative Colitis related to Celiac Disease?**Is Ulcerative Colitis related to Celiac Disease?** Yes. Patients with Ulcerative Colitis have approximately **7 times higher risk** of developing Celiac Disease compared to the general population. This overlap suggests that the **genetic background** and **immune mechanisms** involved in both conditions may share common pathways.
Yes. Patients with Ulcerative Colitis have approximately 7 times higher risk of developing Celiac Disease compared to the general population.
This overlap suggests that the genetic background and immune mechanisms involved in both conditions may share common pathways.
What can I do to feel better?
Is surgery necessary?
Surgery is recommended only when medication and dietary adjustments fail to control the disease.
The main surgical options are:
1. Total Colectomy with Colostomy
a. Removal of the colon, rectum, and anus.
b. Stool is expelled through a stoma (an artificial opening in the abdomen) into a special external bag.
2. Colectomy with Anal Preservation (IPAA – Ileal Pouch-Anal Anastomosis)
c. The surgeon connects the small intestine to the anus, allowing for normal bowel movements.
d. This is the preferred option for younger patients in good overall health.
The decision is made on a case-by-case basis, depending on the severity of the disease, existing complications, and the patient’s general health.
Does Ulcerative Colitis affect fertility?
Not significantly. Most women with Ulcerative Colitis can conceive naturally without major difficulties.
However, if you’re planning a pregnancy, it’s important to inform your gastroenterologist in advance so your medication can be adjusted accordingly.
Some treatments may need to be discontinued or replaced before conception to ensure safety for both mother and baby.
Is Ulcerative Colitis hereditary?
Yes, there is a strong genetic predisposition.
If a family member has Ulcerative Colitis, the risk of developing the disease is significantly higher for first-degree relatives compared to the general population.
Heredity does not guarantee that the disease will occur — but it does mean that increased surveillance and preventive monitoring are strongly advised.
Comprehensive Medical Approach – From Diagnosis to Long‑Term Monitoring
Modern management of Ulcerative Colitis does not only focus on relieving symptoms, but also on controlling inflammation, preventing complications and supporting the patient’s daily functioning. If you experience symptoms such as persistent diarrhea, abdominal pain or blood in the stool — prompt evaluation by a specialist is essential.
Contact Dr. Argyropoulos Theodoros for personalized care and long‑term follow‑up.