IBD – Inflammatory Bowel Disease
Inflammatory Bowel Disease (IBD)
Diagnosis & Treatment
Theodoros Argyropoulos, M.D., M.Sc., Ph.D.
Consultant Gastroenterologist, First Department
General Hospital of Athens “G. Gennimatas”
Scientific Director, Affidea Peristeri Gastroenterology Unit
Contents
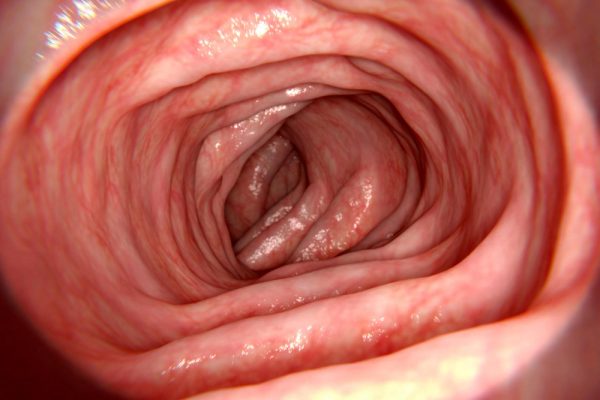
What are Inflammatory Bowel Diseases (IBD)?
Inflammatory Bowel Diseases (IBD) are chronic, immune-mediated conditions that affect the gastrointestinal (GI) tract, causing inflammation, ulcers, and damage to the digestive system. The two main types of IBD are:
Crohn’s Disease, which can affect any part of the GI tract from mouth to anus, often involving deeper layers of the intestinal wall.
Ulcerative Colitis, which is limited to the colon (large intestine) and rectum, affecting only the innermost lining of the bowel.
IBD is not the same as Irritable Bowel Syndrome (IBS), as it involves structural inflammation rather than functional bowel issues. These conditions typically alternate between flare-ups (active symptoms) and remission (minimal or no symptoms) and require long-term monitoring and treatment by a specialist gastroenterologist.

Crohn’s Disease vs Ulcerative Colitis
Key Differences
| Χαρατηριστικό | Νόσος του Crohn | Ελκώδης Κολίτιδα |
|---|---|---|
| Εντόπιση | Από το στόμα έως τον πρωκτό (συχνά ειλεός & παχύ έντερο) | Μόνο στο παχύ έντερο και το ορθό |
| Κατανομή βλαβών | Διακεκομμένη («skip lesions») – φυσιολογικά τμήματα εναλλάσσονται με φλεγμονώδη | Συνεχής φλεγμονή που ξεκινά πάντα από το ορθό |
| Βάθος φλεγμονής | Διατοιχωματική (όλα τα στρώματα του εντερικού τοιχώματος) | Μόνο στο βλεννογόνο και τον υποβλεννογόνιο |
| Μορφολογία | Οίδημα, στενώσεις, συρίγγια, αποστήματα | Συνεχές οίδημα, έλκη, απώλεια αγγείωσης |
| Τυπικές εντοπίσεις | Τελικός ειλεός, ειλεοκολική περιοχή, περιεδρική περιοχή | Ορθό, σιγμοειδές, παχύ έντερο |
| Συχνές επιπλοκές | Στενώσεις, συρίγγια, αποστήματα, δυσαπορρόφηση | Τοξικό μεγάκολο, βαριές αιμορραγίες |
| Αιμορραγία από το ορθό | Λιγότερο συχνή | Πολύ συχνή |
| Εξωεντερικές εκδηλώσεις | Αρθρίτιδα, δερματικές αλλοιώσεις, ραγοειδίτιδα, ηπατοχολική συμμετοχή | Όμοιες, αλλά συχνότερες σε εκτεταμένη νόσο |
| Κίνδυνος καρκίνου παχέος εντέρου | Αυξημένος σε μακροχρόνια/εκτεταμένη νόσο | Αυξημένος σε μακροχρόνια/πανκολίτιδα |
| Κάπνισμα | Αυξάνει τον κίνδυνο και τη βαρύτητα | Παράδοξα προστατευτικό |
| Χειρουργική θεραπεία | Δεν θεραπεύει οριστικά – μπορεί να υποτροπιάσει αλλού | Μπορεί να είναι οριστική (π.χ. ολική κολεκτομή) |
Clinical Significance of the Differences
The distinction between Crohn’s Disease and Ulcerative Colitis determines:
- The treatment strategy (medical, biologic, or surgical)
- The frequency of endoscopic surveillance
- The nutritional and preventive approach
- The prognosis and risk of complications
Crohn’s Disease has a variable course and may relapse even after surgery, while Ulcerative Colitis can be permanently cured when the colon is completely removed.
IBD Symptoms (Inflammatory Bowel Disease)
Common symptoms (in both forms):
- Diarrhea, sometimes with blood or mucus
- Abdominal pain/cramps, bloating
- Fatigue, low-grade fever
- Loss of appetite and weight
- Rectal bleeding
Book an appointment if you experience persistent changes in bowel habits or a combination of the above symptoms lasting more than 2–3 weeks.

Causes & Risk Factors
The exact cause of Inflammatory Bowel Diseases (IBD) has not yet been fully clarified. However, it is now understood that these are multifactorial conditions involving the interaction of genetic, immune, environmental, and microbial factors.
The coexistence of these elements can lead to immune system dysregulation, resulting in chronic inflammation of the intestines.
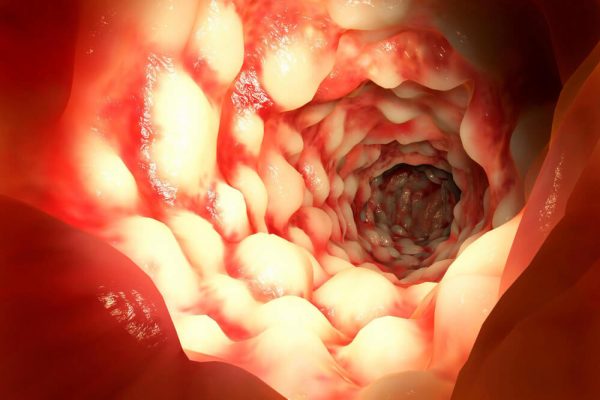
Immune System Dysfunction
In individuals with IBD, the immune system overreacts to microbes or environmental stimuli in the gut.
Instead of protecting the body, it triggers an autoimmune response that causes inflammation in the intestinal wall, damaging healthy tissue.
This results in persistent inflammation, injury to the intestinal mucosa, and alternating cycles of flare-ups and remission.
This chronic inflammatory process is the underlying mechanism in both Crohn’s Disease and Ulcerative Colitis.
Genetic Predisposition
Heredity plays an important role:
Around 15–20% of IBD patients have a family history of the disease.
Several genetic mutations have been identified, such as NOD2/CARD15 in Crohn’s Disease, which affect the immune response to gut microbes.
If one parent has IBD, the risk for the child is 2–8 times higher compared to the general population.
Genetics alone do not cause the disease, but they determine who is more vulnerable to environmental triggers.
Environmental Factors
Lifestyle and environmental conditions play a significant role in the onset and progression of Inflammatory Bowel Diseases (IBD):
Living in northern or urbanized regions: Associated with a higher prevalence of IBD.
Western dietary habits: Diets rich in animal fats and low in fiber are linked to increased intestinal inflammation.
Reduced childhood exposure to microbes: Supports the “hygiene hypothesis,” suggesting that limited microbial exposure may impair immune tolerance.
Stress and psychological pressure: While not direct causes, they can significantly worsen disease flare-ups.
Gut microbiota imbalance (dysbiosis): A reduction in the diversity and balance of beneficial bacteria may promote chronic intestinal inflammation.
These factors do not act alone, but in combination with genetic and immune predispositions, they can trigger or aggravate IBD.
Diagnosis by Dr. Theodoros Argyropoulos
Diagnosis is Combined (Clinical Assessment + Laboratory Tests + Endoscopy ± Imaging):
- Laboratory Tests / Stool Analysis
- Blood Tests & Inflammatory Markers (CRP)
- Fecal Calprotectin (Marker of Intestinal Inflammation)
- Colonoscopy with Biopsies (Gold Standard)
- Direct Visualization of Lesions & Histological Confirmation
- Capability for Therapeutic Interventions When Indicated
- Imaging of the Small Intestine When Needed
- MR/CT Enterography, Ultrasound, and Occasionally Capsule Endoscopy


IBD Complications
Common Complications
- Anemia (Iron and Vitamin B12 Deficiency)
- Weight Loss
- Malnutrition
- Thrombosis
- Dermatologic, Ophthalmologic, and Arthritic Manifestations
- Increased Risk of Colorectal Cancer
Crohn
- Strictures / Obstructions
- Fistulas
- Perianal Abscesses
- Malabsorption
Ulcerative Colitis
- Toxic Megacolon
- Severe Bleeding
Treatment: Medications, Biologic Agents & Management
Goals: Achieve symptom remission, mucosal healing, and prevention of complications.
Personalized Medical Therapy:
- 5-ASA (Aminosalicylates): Mainly for Ulcerative Colitis; mild to moderate disease.
- Corticosteroids: For induction of remission; not for long-term use due to side effects.
- Immunomodulators: Such as thiopurines and others to suppress abnormal immune activity.
- Biologic agents & newer targeted therapies:
- Anti-TNF agents
- Anti-integrin therapies
- Anti-IL-12/23 agents
- Oral small-molecule inhibitors and other targeted treatments
- Antibiotics: In selected situations, e.g., perianal disease or infections.
Treatment is tailored to disease type, severity, and patient response, aiming for long-term disease control and improved quality of life.
Surgery: Last-Resort or for Complications
Immediate management of fistulas/abscesses and strictures (endoscopic dilation in selected cases).

-
Monitoring, Vaccinations & Colorectal Cancer Prevention
Regular monitoring: Track symptoms, CRP/fecal calprotectin, nutritional status, and medication safety.
Vaccinations: Especially recommended before or during immunosuppressive therapy, according to medical guidelines.
Colorectal cancer surveillance: Colonoscopy at individualized intervals for long-standing or extensive disease, typically every 1–3 years after the initial years of disease.
-
Pregnancy, Irritable Bowel Syndrome, Work & Quality of Life
Pregnancy: In most cases, pregnancy is possible. Preconception planning and adjustment of therapy, when necessary, are essential for maternal and fetal safety.
IBD & IBS: These conditions may coexist. Careful differentiation and targeted management ensure appropriate treatment of both.
Lifestyle and Psychological Support: Psychological counseling, regular exercise, and stress management are important allies in maintaining remission and improving quality of life.
Nutrition & Lifestyle (During Flare-Ups and Remission)
There is no single diet for everyone; dietary recommendations should be personalized based on disease type (Crohn’s Disease or Ulcerative Colitis), disease phase (flare-up or remission), and individual food tolerance.
During Flare-Ups:
Mild, easily digestible foods
Adequate fluids and electrolytes
During Remission:
Balanced diet with sufficient protein
Inclusion of fiber as tolerated
Correction of deficiencies (iron, vitamin B12, vitamin D, zinc, etc.)
Foods to Avoid:
Highly processed foods
Excessive alcohol
Other Recommendations:
Smoking cessation, especially important in Crohn’s Disease
Collaboration with a clinical dietitian when needed
Personalized nutrition helps maintain remission, prevent malnutrition, and improve overall quality of life.
Contact Form
The Role of a Specialized Gastroenterologist
Dr. Theodoros Argyropoulos, M.D., M.Sc., Ph.D. has extensive experience in the diagnosis, endoscopic assessment, and long-term management of patients with IBD.
Using a combination of endoscopic, biochemical, and imaging tools, he develops a personalized care plan aimed at:
Mucosal healing
Achieving disease remission without corticosteroids
Preventing complications and hospitalizations
Dr. Argyropoulos organizes the entire strategic plan, including therapy selection based on disease type, location, severity, comorbidities, and patient goals, with close monitoring of clinical, laboratory, and endoscopic markers to optimize outcomes.