Fatty Liver / Hepatic Steatosis
Fatty Liver
Theodoros Argyropoulos, M.D., M.Sc., Ph.D.
Consultant Gastroenterologist, GNA “G. Gennimatas”
Contents
What is Fatty Liver — “Fat in the Liver”
Fatty liver (or “fat in the liver”) is a common condition in which fat (triglycerides) accumulates within liver cells, exceeding 5–10% of the liver’s total weight.
It may be:
Non‑alcoholic (NAFLD – Non-Alcoholic Fatty Liver Disease), the most common form, associated with metabolic syndrome, obesity, diabetes, and elevated lipids, or
Alcoholic, related to chronic alcohol consumption.
The disease may remain benign for years; however, in some patients, it progresses to steatohepatitis (NASH), fibrosis, cirrhosis, or even liver cancer.


How Common Is It?
Fatty liver affects approximately 25% of the general population, while in individuals with obesity or diabetes the rate exceeds 70–80%.
It is currently the most common cause of abnormal liver enzymes in the general population.
Causes and Risk Factors
Fatty liver (steatosis) results from an imbalance between fat intake and fat metabolism in the liver.
The key pathophysiological mechanism is insulin resistance, which leads to increased triglyceride accumulation in hepatocytes and gradually causes inflammation of the liver tissue.
Main Risk Factors:
- Obesity & abdominal fat – the primary cause, especially when visceral fat is present.
- Type 2 diabetes & insulin resistance – promote increased lipogenesis and fat accumulation in the liver.
- Dyslipidemia – high triglycerides, low HDL, and elevated LDL contribute to steatosis.
- Hypertension & metabolic syndrome – aggravate liver inflammation and vascular damage.
- Medications – corticosteroids, tamoxifen, methotrexate, amiodarone, and other hepatotoxic drugs.
- Hormonal disorders – hypothyroidism, polycystic ovary syndrome, hypercortisolism.
- Poor diet & sedentary lifestyle – high intake of sugar, fructose, processed carbohydrates, and trans fats.
- Alcohol – even moderate chronic intake can burden liver metabolism.
- Genetic predisposition – polymorphisms like PNPLA3 and TM6SF2 increase the risk of developing steatosis.
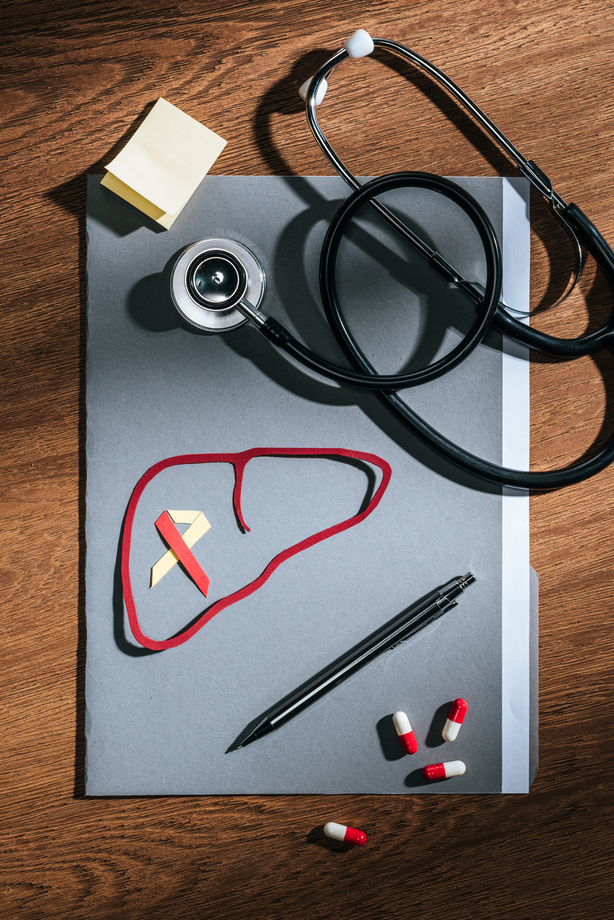
Fatty Liver: Clinical Significance
Fatty liver disease is a multifactorial metabolic condition that reflects the body’s overall metabolic health.
Timely identification and correction of the underlying causes (e.g., blood sugar regulation, lipid levels, weight management, and lifestyle habits) are crucial in preventing progression to steatohepatitis, fibrosis, or cirrhosis.
Symptoms
In its early stages, fatty liver is usually asymptomatic and is often discovered incidentally during an ultrasound or blood test showing mildly elevated transaminases (ALT, AST).
The absence of symptoms does not mean absence of disease — this is why early diagnosis through preventive screening is essential.
-
Mild or Moderate Stages
- Fatigue and a sense of low energy
- General malaise or difficulty concentrating
- Sensation of heaviness or pressure in the right upper abdomen
- Mild hepatomegaly (enlarged liver) during clinical examination
-
Advanced Stages or Complications
- In cases of steatohepatitis, fibrosis, or cirrhosis, the following may occur:
- Jaundice (yellowing of the skin and eyes)
- Ascites (fluid accumulation in the abdomen)
- Swelling in the lower limbs
- Easy bruising or bleeding tendencies
- Confusion or disorientation (a sign of hepatic encephalopathy)
-
Clinical Note
- Fatty liver may remain “silent” for years, until it progresses to NASH or cirrhosis. Monitoring liver enzyme levels and using imaging techniques such as ultrasound or UGAP (Ultrasound-Guided Attenuation Parameter) is the most reliable approach for early diagnosis and prevention.
Fatty Liver: Diagnosis
The diagnosis of fatty liver disease is based on clinical evaluation, laboratory tests, and imaging studies.
A specialized Gastroenterologist–Hepatologist is responsible for the overall assessment, determining the degree of steatosis, and detecting possible inflammation or fibrosis.
Main Diagnostic Steps
Medical history & physical examination
Risk factors are recorded (obesity, diabetes, medications, alcohol consumption), and clinical signs of hepatomegaly or metabolic syndrome are evaluated.
Laboratory tests
Include:
- Transaminases (ALT, AST) and γGT to assess liver function
- Lipid profile, fasting glucose, thyroid hormones
- Exclusion of other liver diseases such as viral hepatitis, hemochromatosis, or autoimmune liver conditions
Liver Ultrasound
The first-line imaging test for diagnosing fatty liver.
- Shows increased echogenicity of liver tissue (the liver appears “brighter” or “whiter” on ultrasound)
- Assesses liver size (hepatomegaly) and the extent of fatty degeneration
- If fat distribution is uneven, the liver is described as having a “geographic pattern”
Advanced Imaging (CT/MRI)
In selected cases, CT or MRI is performed for a more accurate quantitative assessment of steatosis or to exclude other liver pathologies.
A non-invasive examination that measures liver stiffness, providing a reliable estimate of fibrosis severity.
It is an ideal monitoring method for fatty liver disease, eliminating the need for biopsy in most cases.Μη επεμβατική εξέταση που μετρά τη σκληρότητα του ήπατος, παρέχοντας αξιόπιστη εκτίμηση του βαθμού ίνωσης.
Αποτελεί ιδανική μέθοδο παρακολούθησης της νόσου χωρίς την ανάγκη βιοψίας.
Liver Biopsy
Treatment & Management
The management of fatty liver disease is primarily based on lifestyle changes and control of metabolic factors that contribute to fat accumulation in the liver.
The therapeutic approach is individualized by the Gastroenterologist, based on disease stage, coexisting conditions, and the patient’s overall profile.
Key Interventions:
- Weight loss
- Mediterranean-style diet
- Regular physical activity
- Avoidance of toxic factors (e.g. alcohol, hepatotoxic drugs)
- Management of comorbidities (e.g. diabetes, dyslipidemia, hypertension)
- Pharmacotherapy (in selected cases, under specialist guidance)
- Bariatric surgery (in cases of morbid obesity)
- Liver transplantation (in end-stage liver disease)

Adults over 45 years old, as well as those with obesity, diabetes, high cholesterol, or hypertension, are advised to undergo annual blood tests and liver ultrasound.
The combination of basic lab work and ultrasound can detect the disease before it causes irreversible liver damage.
When to See a Specialist Gastroenterologist
Fatty liver can silently progress and cause significant liver damage without obvious symptoms.
Timely monitoring by a specialized Gastroenterologist – Hepatologist is crucial to prevent complications and achieve full disease reversal.
Seek immediate consultation if you have:
- Obesity, type 2 diabetes, high lipid levels, or a history of metabolic syndrome
- Elevated transaminases or other abnormal liver test results
- Ultrasound findings suggestive of steatosis
- Jaundice, abdominal fluid (ascites), swelling, or confusion
- Regular alcohol consumption or use of medications that may affect the liver
Also contact a specialist if you notice:
- Yellowing of the skin or eyes (jaundice)
- Swelling in the abdomen, legs, or ankles
- Difficulty concentrating, drowsiness, or behavioral changes
- Vomiting blood or black stools (signs of advanced disease)
Early diagnosis and regular follow-up can prevent progression to steatohepatitis, fibrosis, or cirrhosis and may lead to complete reversal of liver damage.
Frequently Asked Questions (FAQ)
Is fatty liver reversible?
Does “fatty liver” cause pain?
What is the most reliable test?
Liver ultrasound is the first-line imaging test.
For precise staging, UGAP and FibroScan® provide non-invasive, reliable assessment of steatosis and fibrosis.
Can I drink alcohol?
Abstinence or strict limitation is recommended, especially in cases of steatohepatitis (NASH) or fibrosis.
How often should I get checked?
What lifestyle changes help?
- Adopt a Mediterranean diet and reduce salt, sugar, and refined carbs
- Engage in regular physical activity (walking, cycling, swimming)
- Avoid smoking and alcohol
- Get vaccinated against hepatitis A & B, influenza, and pneumococcus
- Do not take supplements or herbs without medical guidance
Is fatty liver dangerous?
If left untreated, it can progress to steatohepatitis (NASH), fibrosis, cirrhosis, or, in rare cases, hepatocellular carcinoma.
The disease is also linked to increased cardiometabolic risk, as it is associated with hypertension, diabetes, and atherosclerosis.
What about cost and duration of the exam?
The exam typically lasts 10–15 minutes, while the cost depends on the type of procedure (diagnostic or therapeutic) and the facility where it is performed.
Book an Appointment
Fatty liver disease is common — but reversible if diagnosed early and managed with a holistic approach.
Fatty liver is not always harmless. Even in the absence of symptoms, it signals an underlying metabolic dysfunction that affects the entire body.
Prevention, early diagnosis, and regular medical monitoring by a specialist gastroenterologist can stop disease progression and ensure complete restoration of liver function.
A Gastroenterologist–Hepatologist is the appropriate medical specialist for thorough evaluation, personalized guidance, and long-term follow-up.